Obstructive Sleep Apnoea - What it is & How it is treated
Table of Contents
What is Obstructive Sleep Apnoea (OSA)?
Apnoea (also spelt apnea) means “without breathing”
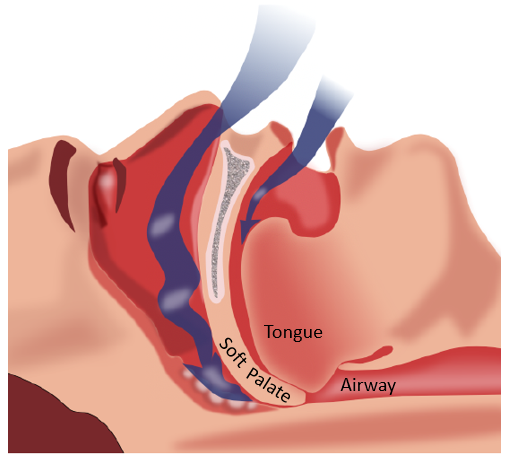
In the condition of Sleep Apnoea, a person can repeatedly have short periods during sleep when he/she stops breathing. This happens when the muscles at the throat relax and collapse, the tongue falls back and the airway is blocked or obstructed.
When the airway is blocked this way, breathing stops and carbon dioxide builds up in the body. The brain rouses the person from sleep enough for the person to gasp for air and normal breathing is restored. The person then falls back into sleep, only for this to happen again.
Most people with sleep apnea do not know they have it because they do not wake up enough to realize it. The condition is most often observed by their partners.
Obstructive Sleep Apnoea (OSA) can be accompanied by snoring and/or grinding of the teeth — a condition that is also known as bruxism.
There are other types of apneas but this article will focus on obstructive sleep apnea (OSA) as it is the most common type.
Is Obstructive Sleep Apnoea (OSA) dangerous?
The repeated interruptions in breathing during obstructive sleep prevent you from getting enough oxygen. The amount of restful, healing sleep you get every night is limited. Not only would you wake up not feeling rested, but you may feel sleepy during the day, dozing off unexpectedly, for example, while driving. Over time, sleep apnea will impact your general physical & mental health.
OSA has been associated with cardiovascular diseases such as:
– Hypertension (high blood pressure)
– Stroke
– Myocardial ischemia (heart attacks) and also Type II Diabetes.
What are the risk factors for Obstructive Sleep Apnea
(OSA)?
Being overweight – Excess fat around the neck may constrict the airway. Sleep apnea occurs in about 3 percent of normal weight individuals but affects over 20 percent of obese people.
Neck circumference – People with thicker necks might have narrower airways.
Alcohol and sedating drugs These substances relax the muscles in your throat, which can make you more likely to have obstructive sleep apnea.
Smoking – Smokers are three times more likely to have obstructive sleep apnea than are people who have never smoked. Smoking can increase the amount of inflammation and fluid retention in the upper airway
Narrowed airway – Enlarged tonsils or adenoids can block the airway, particularly in children.
Small lower jaw that is retruded or set back relative to the upper jaw may result in a narrow airway.
Age – Sleep apnea occurs significantly more often in older adults.
Men – are 2 to 3 times more likely to have sleep apnea than are women. However, women increase their risk if they’re overweight or if they’ve gone through menopause.
Nasal congestion – If you have trouble breathing through your nose — whether from an anatomical problem or allergies — you’re more likely to develop obstructive sleep apnea.
Medical conditions – Polycystic ovary syndrome, hormonal disorders, prior stroke and chronic lung diseases such as asthma can make an individual more prone to developing OSA.
Sleeping on your back – Lying on your back may make you more likely to have the tongue fall back against your soft palate and back of the throat, blocking off air from entering your lungs. (See the diagram below)
What are the signs that I could be having OSA?
- Waking up tired, even after a full night’s sleep
- Waking up frequently during the night, for no apparent reason.
- Waking up with a headache
- Feeling sleepy or tired during the day.
- Having problems with memory or concentration
- Snoring
- Your partner notices you gasping or pausing your breathing while you sleep.
- Dental problems associated with sleep apnea include jaw-joint(TMJ) disorders, bruxism, and mouth breathing.
How is a diagnosis of Obstructive Sleep Apnoea made?
The Dentist can often identify a person with risk factors for sleep apnoea and can detect the dental problems associated with it e.g. bruxism. For the dental treatment of such conditions to be effective, the underlying sleep apnea needs to be controlled.
The diagnosis of Obstructive Sleep Apnoea has to be made by a medical doctor like an ENT (Ear, Nose & Throat) doctor or a respiratory physician. Such doctors can order a sleep test to determine the presence and severity of OSA.
The long-term success of your dental treatment will depend on the effective control of OSA
How can Obstructive Sleep Apnoea (OSA) be treated?
Treatment would depend on the severity of the condition.
For very mild cases, the following would be the first steps.
- Lose weight – as obesity is strongly associated with OSA, losing weight would be a good first step. Weight loss would also help to manage snoring
- Sleep position – as sleeping on the back causes the tongue and jaw to fall back, sleeping on the side would help. Or, elevate the upper body during sleep Again, this would help to reduce snoring.
- Treat Allergies or other causes of nasal or sinus congestion
- Stop smoking
- Avoid alcohol
- Exercise & sleep hygiene
– Have a ritual of “winding down for the day” with gentle exercise and meditation
– Sleep in a dark, cool room away from computers and phones. Make your body and mind ready for sleep.
If the OSA is considered more worrisome, the following may be recommended.
- Positive Airway Pressure Devices – This is the first line of treatment, particularly for moderate to severe cases of OSA. They can be effective if used correctly. There are several versions of such devices. The most common is the CPAP (Continuous Positive Airway Pressure) device. It comprises a machine that takes in room air, filters it, and delivers the air at the prescribed pressure via a tube to a face mask worn during sleep.

It is necessary to work with a sleep technician or respiratory therapist to check on matters like how well the mask is fitting, dryness or congestion of the nose, whether there is any air leakage and ensure the appropriate air pressure is delivered to control your apnoea. Here is an excellent video by the Cleveland Clinic: https://cdnapisec.kaltura.com/index.php/extwidget/preview/partner_id/2207941/uiconf_id/37292221/entry_id/1_vxgg8qxd/embed/dynamic
- Oral Appliances may be prescribed for those diagnosed with mild to moderate OSA, especially if they have difficulty adapting to the CPAP device or simply want a less cumbersome appliance.
Oral appliances are small enough to fit into the palm of your hand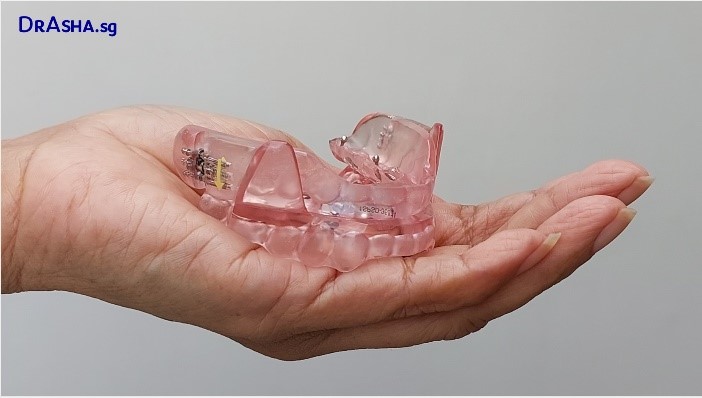
There are many designs of oral appliances. All of them are designed to hold the lower jaw forward. This helps to keep the tongue from falling back. It can be effective in controlling apnoea and snoring as well.
The appliances usually come in two parts, one part fits over the upper teeth and the other part fits over the lower teeth.

Oral appliances are custom-made by dentists.
Constructing the appliance normally takes just two visits. The appliance can be adjusted to keep the lower jaw forward to a lesser or greater degree to adequately control the apnoea.
Regular checks are needed to ensure fit is maintained and the appliance & supporting teeth are in good condition.

Other treatment options:
- Nerve Stimulation is a new idea where the nerve controlling the tongue muscle is stimulated to keep a forward position. It is not yet available in Singapore.
- Surgery – there are many surgical procedures to modify the tissues around the throat. These may be helpful in reducing snoring but the long-term efficacy in apnoea control is not always predictable.
Please see the separate article here
Summary
Obstructive Sleep Apnoea (OSA) is a condition with serious consequences.
Dentists may be the first healthcare provider to alert you to this condition.
If there is a suspicion of OSA, have yourself examined by a physician and get a diagnosis. So many aspects of your health depend on it.
